Comparing the medical plans
The chart below serves as a side-by-side comparison of the medical plans that Corewell Health offers through Priority Health. Your primary address in Workday drives available medical plan options*.
You have the choice between two types of plans:
- The HMO which is a first dollar, co-payment plan where you are not subject to the deductible for services unless they are hospital-based services in which you will pay a smaller deductible up to a maximum out of pocket. This plan’s premiums are higher because of this lower cost at time of services.
- The HDHPs which are high deductible medical plans where you must meet the deductible prior to any co-insurance or co-payments under these plans, including prescriptions. These plans’ premiums are lower because of this higher cost out of pocket. Both of the Corewell Health HDHPs offer the same plan design; the only difference is that the HDHP-POS plan offers coverage outside of the Corewell Heath and Priority Health networks. These plans are health savings account (HSA bank account) eligible with contributions to the account from Corewell Heath to offset some of your deductible.
The HDHP-POS is the only plan available to team members living in the Upper Peninsula of Michigan.
**For details regarding providers and services for your plan, see below.
***Annual Corewell Health employer HSA contribution is deposited into the HSA account each paycheck (approx. $19.23 per pay for single and $28.75 per pay for all other coverage tiers until the maximum has been reached).
Tier 2 services that apply to the deductible will credit both Tier 1 and Tier 2 deductibles. Only Tier 1 services will credit Tier 1 deductibles. Tier 1 and Tier 2 out-of-pocket maximums track in combination. On the HDHP-POS plan, Tier 3 does not apply to Tier 1 or Tier 2. The HDHP-HMO plan provides a similar network as the HMO plan and does not include coverage for out-of-network providers.
HMO Plan
This plan offers higher premiums and lower out-of-pocket costs. Costs are lowest when members receive care at Corewell Health facilities and providers; there is no out-of-network coverage.
HDHP-HMO and HDHP-POS Plans
The high-deductible health plans balance lower premiums with higher out-of-pocket costs and out-of-network coverage. Corewell Health helps offset these costs when you fund a Health Savings Account.
Medical benefit providers and service areas
The medical benefit plans offer a tiered structure to give you coverage, flexibility and access based on where you work and live, where you choose to receive your care and the provider you select. When accessing care within Corewell Health and other affiliated providers/facilities you are able to save on the out-of-pocket cost of this care.
Your home address in Workday will determine the provider tiers and cost you will pay based on the facilities or providers you seek for services.
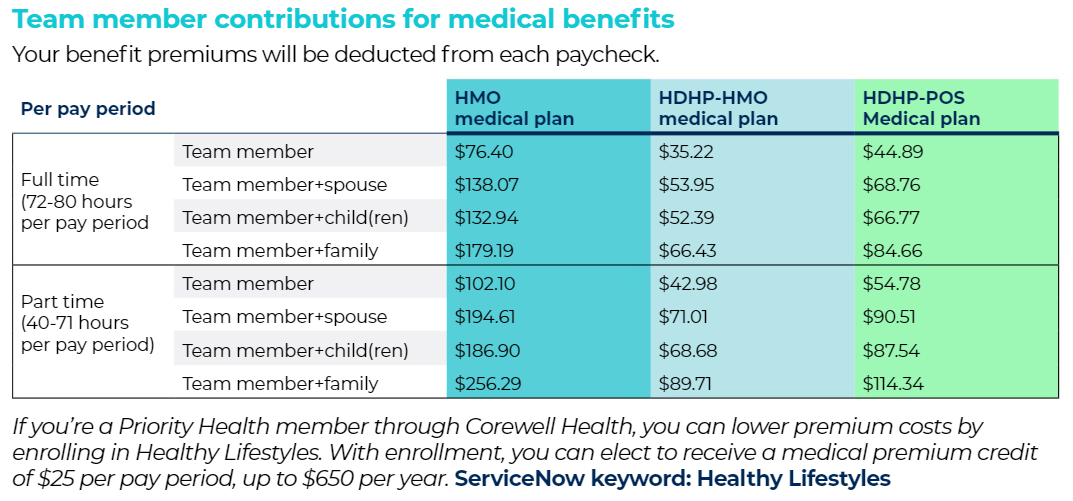
Team member contributions
Navigating Tiers In Your Medical Plan
What Happens If My Primary Care Doctor Is In Tier 2?
What Happens If I Need A Hospital-based Service (like an X-Ray?)
What Happens If I Need Hospitalization?
Priority Health HMO
Priority Health HDHP
Find your Provider
To find in-network providers under your plan, visit priorityhealth.com.
First, select the Find a Doctor tool. Under the employer plan section, select Corewell Health Employer Group.
Out-of-area team members: Select the Find a Doctor tool. Under the plan dropdown menu, select:
- PriorityHMO for the HMO and HDHP-HMO Plans
- PriorityPOS A for the HDHP-POS Plan
- Cigna for members out of state
Riders on the Corewell Health Medical Plan
Expanded infertility rider
Currently, all Priority Health medical plans cover diagnostic, counseling, and planning services for the treatment for the underlying cause of infertility and prescription drugs used for the purpose of treating infertility. Examples of covered services include endometrial biopsy, diagnostic laparoscopy or hysteroscopy, hormone evaluation, and semen analysis.
The expanded infertility rider provides coverage for assisted reproduction and artificial conception services regardless of provider participation. Examples of covered assisted reproduction and artificial conception services include within the expanded rider: Sperm count, egg freezing, thawing and storage, in vitro fertilization (IVF), artificial insemination (AI) and services associated with the treatment and underlying conditions of assisted reproduction and artificial conception such as ultrasounds and imaging. Services specific to this rider have a $50,000 lifetime maximum benefit.
Habilitation coverage rider
This rider provides coverage for habilitation services which are defined as those health care services that help a person keep, learn, or improve skills and functioning for daily living e.g., therapy for a child who isn’t walking or talking at the expected age.
All of the following must be met for coverage of habilitative services not related to autism spectrum disorder:
- Treatment must be evidence-based physical or occupational therapy provided by an appropriately licensed therapist under the direction of a physician or advanced practice nurse in accordance with a written treatment plan established or certified by the treating physician or advanced practice nurse.
- One of the following diagnoses:
- Developmental delay
- Developmental coordination disorder
- Mixed developmental disorder
- Developmental speech or language disorder
Lab coverage for CBC, CMP and Vitamin D
CBC, CMP and/or vitamin D labs at 100% prior to deductible with the HMO plan and 100% after the deductible with the HDHP plans.
Chronic Conditions Rider for Prescriptions
Specific to the HDHP medical plans, this rider allows those with a chronic condition such as asthma, cholesterol, depression, diabetes, heart conditions, and/or osteoporosis to get certain defined medications at co-payments before the deductible needs to be met.
Obesity Medication Rider for Prescriptions
A rider for prescription medication related to obesity treatment is covered by our medical plans (after deductible with the HDHP plans). As with all other prescription medications, the medication must be on the Priority Health formulary.
Cranial Prosthesis Rider
This coverage rider provides coverage for cranial prosthesis for hair loss due to a medical condition as described in the Priority Health schedule of copayments and deductibles. Cranial prosthesis (wig, toupee, headband) is covered when performed by a health professional.
ServiceNow keyword: medical plans
Finding a Priority Health Provider
To find in-network providers under
your plan, visit priorityhealth.com.
First, select the Find a Doctor tool. Under the employer plan section, select Corewell Health Employer Group.
Out of area team members: Select the Find a Doctor tool. Under the plan dropdown menu, select:
- PriorityHMO for the HMO and HDHP-HMO Plans
- PriorityPOS A for the HDHP-POS Plan
- Cigna for members out of state
Finding a Corewell Health Provider
For a complete list of Corewell Health facilities, visit corewellhealth.org and scroll to "Our connected network of care." From there, you can select a region.
You are able to obtain services from either side of the system at Tier 1 coverage.